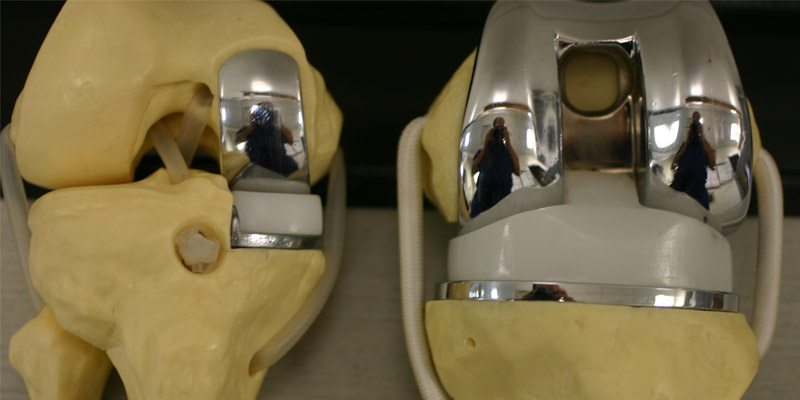
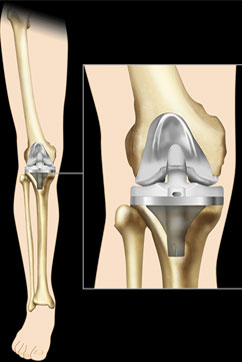
Yes, primarily there are two kinds of Knee replacement surgeries TKR (Total Knee Replacement) and UKR (Unicondylar / Partial Knee Replacement). Knee Replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee joint. This is termed as Implant or Prosthesis.
Knee Revision Surgery
Knee revision surgery, which is also known as revision total knee arthroplasty, is a procedure in which the previously implanted artificial knee joint, or prosthesis is removed. It is replaced with a new prosthesis. Knee revision surgery may also involve the use of bone grafts. The bone graft may be an autograft, which means that the bone is taken from another site in the patient’s own body; or an allograft, which means that the bone tissue comes from another donor.
Situations in Which TKR is helpful
1. Pain that limits activities such as walking, climbing stairs and getting in and out of chairs, or even moderate or severe knee pain at rest.
Why THR?
Osteoarthritis of the hip joint is the most common reason for people opting in favor of Hip Replacement surgery. Hip Replacement is an option worth considering if there is severe pain, loss of motion or deformity of the hip joint. Hip replacement is also used in people with hip injuries, rheumatoid arthritis and other medical conditions, such as a bone tumor or bone loss due to insufficient blood supply (avascular necrosis).
Before the surgery, an Orthopaedic surgeon will counsel the patient in person and carry out examination and evaluation. The surgeon will thoroughly check the patient’s medical history so as to ensure that the patient is healthy enough to undergo surgery. The surgeon will physically examine the hip, paying attention to the range of motion in your joint and the strength of the muscles around the hip. Blood tests, an X-ray or other radiological investigations are routine procedures that may be required.
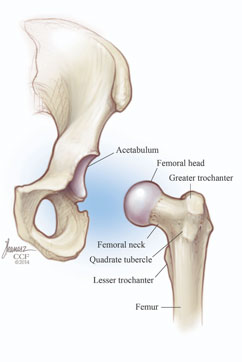
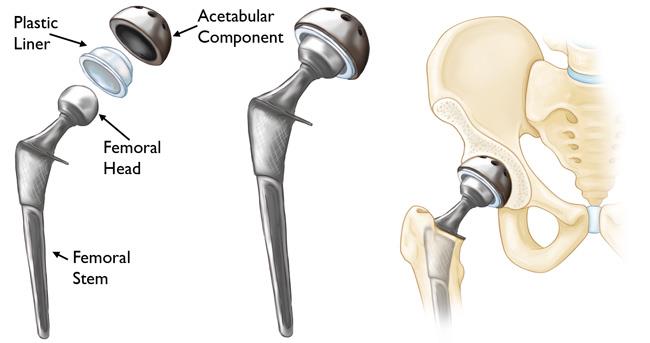
This preoperative evaluation is a good opportunity to ask questions and doubts if any about the procedure. The hip is a ball and socket joint, linking the “ball” at the head of the thigh bone (femur) with the cup-shaped “socket” in the pelvic bone ( as seen in the image below). A total hip prosthesis is surgically implanted to replace the damaged bone within the hip joint.